NIH HEAL Initiative Research: Making a Difference
The NIH HEAL Initiative® is a research effort that combines the power of science and community to address the evolving public health challenge of poorly treated pain, opioid misuse, addiction, and overdose.
HEAL-funded research is making a difference in the lives of individuals and communities across America. This important work relies on strong partnerships with federal agencies, the private sector, research institutions, and communities.
We are all working together to help end addiction long-term: the vision for the NIH HEAL Initiative.
Download a PDF of the NIH HEAL Initiative: Making A Difference e-Pub.

HEAL Research: Pain Coping Skills Training Decreases How Much Pain Affects Daily Life for People With Dialysis-Dependent Kidney Failure
The Problem: Chronic pain is an ongoing struggle for many people undergoing dialysis for kidney failure. Pain often gets in the way of daily life and affects mood and quality of life. Pain treatment options are limited for people with dialysis-dependent kidney disease who are more likely to have worse side effects from opioids, a common pain treatment for these individuals, making it a challenge to manage pain. Effective alternatives or additions to pain medications are desperately needed.
New Finding: The Hemodialysis Opioid Prescription Effort (HOPE) Consortium Trial to Reduce Pain and Opioid Use in Hemodialysis, funded by the NIH HEAL Initiative, showed that a cognitive behavioral-based pain coping skills training significantly decreased how much pain interfered with daily life in people with dialysis-dependent kidney failure. Study participants reported improved physical function, reduced depression symptoms, and less intense pain compared to those receiving usual care.
Imagine the Future: With new non-pharmacologic, non-invasive strategies like pain coping skills training for managing pain, people with dialysis-dependent kidney failure can more easily participate in daily activities, and experience less intense pain and depression and improved quality of life.
- HEAL Project: Hemodialysis Opioid Prescription Effort (HOPE) Consortium Trial to Reduce Pain and Opioid Use in Hemodialysis
- Publication: Pain coping skills training for patients receiving hemodialysis: The HOPE Consortium randomized clinical trial
- HEAL Researcher: Laura M. Dember, M.D., University of Pennsylvania
- Press Release: Behavioral intervention decreases how much pain affects daily activities in people with dialysis-dependent kidney failure

HEAL research: Better Ways to Model Pain in the Lab
The Problem: To learn about what causes pain in the body, scientists need better ways to model pain in the lab. Often, researchers model pain in the lab by studying cells in a dish. Even though scientists know that several different types of cells in the brain are involved in pain, most cell models in the lab focus on the role of only one cell type: neurons.
New Finding: HEAL researchers have created a new way to model pain in the lab that uses both neurons and another type of brain cell called astrocytes. Because the new model uses more than one type of cell, it is more similar to how pain really works in the body. If scientists use the new model to test pain therapies, there is a better chance that the therapies will work in the human body.
What Does This Mean for the Future of Pain Care? Testing pain medications in cell models could help researchers create powerful, non-addictive treatments for chronic pain.
- HEAL Project: Translational Research to Advance Testing of Novel Drugs and Human Cell-Based Screening Platforms to Treat Pain and Opioid Use Disorder
- Publication: Electrically-evoked Oscillating Calcium Transients in Mono- and Co-cultures of iPSC Glia and Sensory Neurons
- HEAL Researcher: Bryan James Black, Ph.D., University of Massachusetts – Lowell
HEAL research: Researchers identify individual chronic pain signatures in the brain
The Problem: For the millions of Americans living with chronic pain, the experience is unique in every individual. Currently available treatments do not provide adequate relief, and new non-addictive and effective medications are desperately needed. The development of new medications for pain has significantly declined over the past decade. A major hurdle is the ability to accurately measure chronic pain, in order to test new treatments.
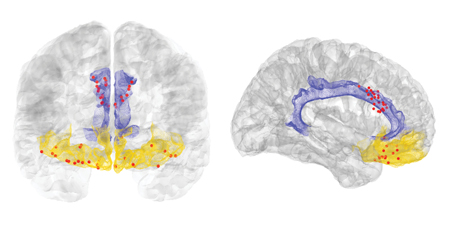
New Finding: For the first time, HEAL-funded researchers measured pain-related brain activity in real time from inside the brains of people with chronic pain disorders caused by stroke or amputation. The scientists measured pain signals in regions of the brain associated with pain perception as well as the emotional response to pain.
Imagine the Future: Chronic pain signatures that measure pain episodes in individuals in real time lead to personalized approaches to effective, non-addictive pain management.
- HEAL Project: Multisite Adaptive Brain Stimulation for Multidimensional Treatment of Refractory Chronic Pain
- Publication: First-in-human prediction of chronic pain state using intracranial neural biomarkers
- HEAL Researcher: Prasad Shirvalkar, Ph.D., University of California, San Francisco
- Press release: Brain signatures for chronic pain identified in a small group of individuals

HEAL research: Healthy developmental paths for babies exposed to opioids
The Problem: In the United States, an infant is diagnosed with neonatal opioid withdrawal syndrome (NOWS) about every half hour. NOWS symptoms typically appear in the first few days of life and include irritability, tremors, poor sleeping, and difficulty feeding – and babies can be hospitalized in the neonatal intensive care unit for several days to weeks.
New Finding: HEAL researchers through the Advancing Clinical Trials in Neonatal Opioid Withdrawal (ACT NOW) program show that using the Eat, Sleep, Console (ESC) care approach can cut hospital stays for babies experiencing withdrawal symptoms and reduce their need to receive medication as part of their treatment.
Imagine the Future: Infants exposed to opioids during pregnancy have a healthy developmental path to childhood and beyond.
- HEAL Project: Advancing Clinical Trials in Neonatal Opioid Withdrawal
- Publication: Eat, Sleep, Console Approach or Usual Care for Neonatal Opioid Withdrawal
- HEAL Researchers: Leslie Young, M.D., University of Vermont; Lori Devlin, D.O., University of Louisville School of Medicine; Stephanie Merhar, M.D., University of Cincinnati
- Press Release: “Eat, Sleep, Console” reduces hospital stay and need for medication among opioid-exposed infants

HEAL research: Buprenorphine in the emergency department is safe and effective in the era of fentanyl
The Problem: Fentanyl and other synthetic opioids have created a deadly landscape for people who use drugs. Clinical guidelines that recommend emergency department-administered buprenorphine to treat opioid use disorder are underused in part because providers fear it will cause the rapid and marked onset of painful withdrawal symptoms after the first dose of buprenorphine.
New Finding: HEAL-funded research through the National Institute on Drug Abuse now shows that only a fraction of people with opioid use disorder whose drug use includes fentanyl (under 1%) experienced withdrawal after being prescribed buprenorphine in the emergency department. The findings are a key step toward affirming the safety and effectiveness of emergency department-administered buprenorphine that includes screening, treatment, referral, and follow-up.
Imagine the Future: Emergency departments across America routinely provide life-saving medication and resources for people at risk for overdose.
- HEAL Project: Emergency Department-INitiated bupreNOrphine and VAlidaTIOn Network Trial (ED-INNOVATION)
- Publication: Incidence of Precipitated Withdrawal During a Multisite Emergency Department–Initiated Buprenorphine Clinical Trial in the Era of Fentanyl
- HEAL Researcher: Gail D’Onofrio, M.D., M.S., Yale School of Medicine
- Press Release: Buprenorphine initiation in the ER found safe and effective for individuals with opioid use disorder who use fentanyl
Stay Connected
Stay up to date on the latest HEAL Initiative research advances by subscribing to receive HEAL content directly to your inbox.
 U.S. Department of Health & Human Services
U.S. Department of Health & Human Services
