Discovery and Validation of Novel Targets for Safe and Effective Treatment of Pain
Overview
The Research Need
Pain is a major factor in many acute and chronic conditions, but only a small number of new therapeutics for pain advance from early stage (Phase 1) clinical trials to approval by the U.S. Food and Drug Administration. There is an urgent need for innovative approaches to find and validate new biological targets for treating pain, as well as for new animal models to test the effectiveness of new medications on these targets.
About the Program
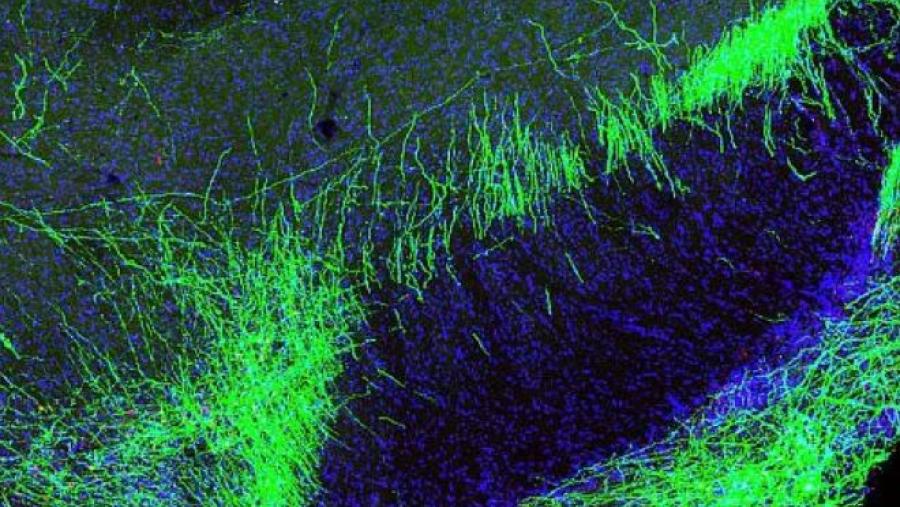
This program aims to identify new, non-addictive biological targets in the peripheral and central nervous systems, as well as in the immune system and other body organs and tissues involved in detecting and transmitting pain signals. The research also explores understudied genes and proteins (the “druggable” genome and proteome) associated with pain, pain perception, and opioid use disorder that might serve as markers or targets for treatment.
To validate targets, this research employs knockout animals or human tissue and supports independent replication of results. The program identifies and validates small molecules and biologics (such as antibodies and cell-based therapies) that could lead to translational research to develop pain therapeutics. The program also develops, characterizes, and validates animal models of pain and develops reliable pain outcome measures. That includes both rodents and animals that are more similar to humans in size, anatomy, and physiology.
PRECISION Human Pain Network
Within this program, the Program to Reveal and Evaluate Cells-to-Gene Information that Specify Intricacies, Origins, and the Nature of Human Pain (PRECISION Human Pain) network focuses on research efforts to identify and describe mechanisms underlying pain experiences in humans rather than animal models. The PRECISION network coordinates, curates, harmonizes, and integrates comprehensive datasets generated from this research. The network’s human-focused research capitalizes on recent technological advances to study human tissues and cells involved in pain processing. A key goal is to identify molecular signatures, cell types, and cellular function signatures that underlie human pain pathways. These activities will enable future translational research and the development of non-addictive pain therapies for human pain conditions.
Open Funding Opportunities
There are no Open Funding Opportunities at this time.Research Examples
Research examples supported by this program include:
- Determining the contribution of peptidase inhibitor 16 to chronic pain using mouse models and human tissues
- Evaluating the role of molecular interactions on spinal cord sensitization, excitatory synapse formation, and pain state development in models of neuropathic pain
- Validating vascular endothelial growth factor receptors 1 and 2 as novel therapeutic targets for osteoarthritis pain
- Determining mechanisms of activation of sympathetically mediated sensory neurons thought to be involved in spontaneous pain
- Developing a range of non-rodent animal models of pain
- Identifying animal behaviors and other outcomes that can be used to measure pain
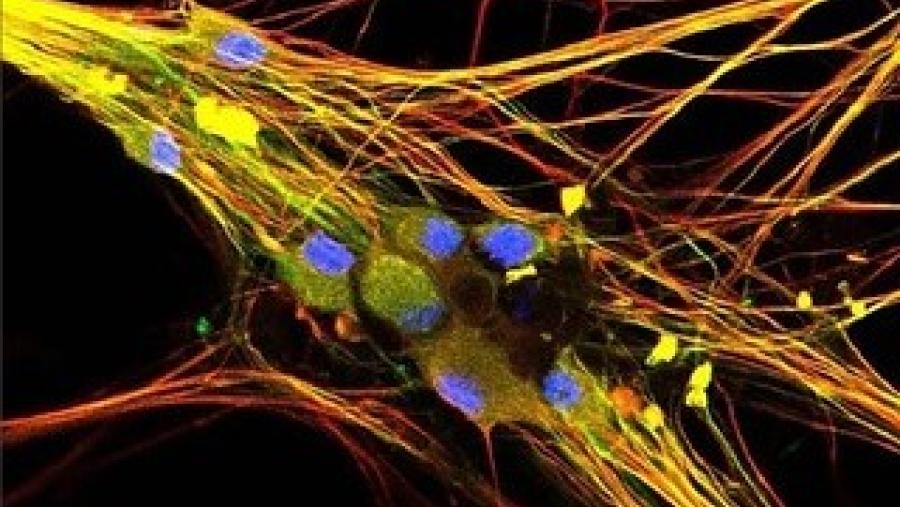
- Analyzing individual human cells to determine how human pain receptors communicate pain signals throughout the nervous system
- Analyzing gene expression of individual cells in pain nerve cell clusters in individuals with and without pain
- 4E Therapeutics Inc. – Texas
- Brigham and Women's Hospital – Massachusetts
- Columbia University Health Sciences – New York
- Drexel University – Pennsylvania
- Duke University – North Carolina
- Ichan School of Medicine at Mount Sinai – New York
- Johns Hopkins University – Maryland
- New York University – New York
- Northwestern University – Illinois
- Palo Alto Veterans Institute for Research – California
- Research Triangle Institute – North Carolina
- Rutgers Biomedical and Health Sciences-New Jersey Medical School – New Jersey
- Rush University Medical Center – Illinois
- Stanford University – California
- State University of New York at Buffalo – New York
- St. Louis University – Missouri
- The University of Texas, Dallas – Texas
- The University of Texas MD Anderson Cancer Center, Houston – Texas
- University of Arizona – Arizona
- University of California, Irvine – California
- University of California, San Diego – California
- University of California, San Francisco – California
- University of Cincinnati – Ohio
- University of Illinois, Chicago – Illinois
- University of Iowa – Iowa
- University of Maryland, Baltimore – Maryland
- University of Minnesota – Minnesota
- University of North Carolina, Chapel Hill – North Carolina
- University of Pittsburgh – Pennsylvania
- University of Texas Health Science Center at San Antonio – Texas
- Washington University – Missouri
Contact
Michael L. Oshinsky, Ph.D., NINDS
D.P. Mohapatra, Ph.D., NINDS
Participating NIH Institutes, Centers, and Offices
- Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD)
- National Cancer Institute (NCI)
- National Center for Advancing Translational Sciences (NCATS)
- National Center for Complementary and Integrative Health (NCCIH)
- National Eye Institute (NEI)
- National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS)
- National Institute of Dental and Craniofacial Research (NIDCR)
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK)
- National Institute of Neurological Disorders and Stroke (NINDS)
- National Institute of Nursing Research (NINR)
- National Institute on Aging (NIA)
- National Institute on Alcohol Abuse and Alcoholism (NIAAA)
- National Institute on Drug Abuse (NIDA)
- National Library of Medicine (NLM)
View Other Research Programs in This Focus Area
- Development and Optimization of Non-Addictive Therapies to Treat Pain
- Integrated Basic and Clinical Team-Based Research in Pain
- Preclinical Screening Platform for Pain (PSPP)
- Restoring Joint Health and Function to Reduce Pain Consortium (Re-JOIN)
- Translating Discoveries into Effective Devices to Treat Pain
- Translational Research to Advance Testing of Novel Drugs and Human Cell-based Screening Platforms to Treat Pain and Opioid Use Disorder
 U.S. Department of Health & Human Services
U.S. Department of Health & Human Services