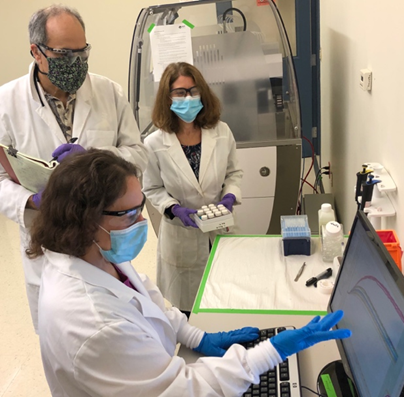
Knopp scientists Kelly Picchione, Ph.D. (foreground), Armando Signore, Ph.D. (back left), and Lynn Resnick, Ph.D. (back right), are in the laboratory reviewing results from assays testing compounds on Kv7.2/3 channels. Image courtesy of Thomas Petzinger, Jr., Knopp Biosciences LLC
Unbearable. Relentless. Stabbing. Like electric shocks.
That’s how people with nerve pain, also called neuropathic pain, describe how it feels. Up to 1 in 10 people suffer from chronic neuropathic pain, and diabetes is the most common cause. High blood sugar can injure nerves, most often in the legs and feet.
Few effective medicines are available to treat this intense pain, but sometime opioid medicines are used, presenting risks of misuse and addiction.
With funding from the Helping to End Addiction Long-term® Initiative, or NIH HEAL Initiative®, a team of researchers at Knopp Biosciences LLC in Pittsburgh, Pennsylvania, is taking on the challenge of developing a new nonaddictive treatment for neuropathic pain, beginning with diabetic neuropathies.
The multi-year project is funded under the NIH HEAL Initiative’s program dedicated to Optimizing Non-Addictive Therapies to Treat Pain. The program’s goal is to discover and develop novel treatments for chronic pain that have fewer side effects and lower risks of misuse or addiction.
Senior research investigators Lynn Resnick, Ph.D., and Armando P. Signore, Ph.D., along with Kelly Picchione, Ph.D., group leader, are directing the project Selective Kv7.2/3 Activators for the Treatment of Neuropathic Pain. Resnick is a medicinal chemist with years of experience in designing and identifying potential new drugs. Signore and Picchione have backgrounds in neuroscience and expertise in developing ways to test compounds for effectiveness.
The Knopp team spoke with us about their project.
Why is effective pain management important for overcoming the opioid epidemic?
Doctors sometimes prescribe opioids for neuropathic pain, especially if other medications don’t work. But opioid medications are often not effective in treating chronic neuropathic pain, and people can become dependent on opioids, misusing them or even turning to illicit opioids, which are often more potent and can be deadly.
Identifying a safe, non-addictive alternative to opioids for pain management is critical for addressing the opioid crisis.
What’s the basic problem that causes neuropathic pain?
Neuropathic pain is most often caused by disease, such as diabetes; by injury, such as a herniated disk in the spine; or by infection, as in shingles. The pain begins when nerves are damaged and don’t function normally, causing abnormal patterns of electrical activity in nerve cells. Our brains interpret these irregular signals as pain, even if there’s no painful stimulus. For that reason, nerve pain is hard to target with medications.
The focus of your project is on neuropathic pain associated with diabetes. What is diabetic neuropathic pain? Why do we need new treatments for this condition?
People who have diabetic neuropathic pain say it feels like burning, stabbing, or shooting pains most often starting at their fingertips or toes. Symptoms are often worse at night, making it difficult to get a good night’s sleep. Sometimes even the light touch of clothes or bedsheets can be painful. To deal with this intense, nonstop pain, many patients rely on opioid medications for relief. But this comes at a high risk due to the addictive potential of opioids.
The problem of diabetic neuropathic pain is only going to get worse. Right now, one out of 10 Americans has diabetes. Worldwide, it’s likely that more than 350 million people will have the condition by 2030 — that’s twice as many as in 2000. This means that even more people could become dependent on opioids as they seek relief from hard-to-treat diabetic neuropathic pain. We view the need for new options for treating diabetic neuropathic pain as a significant and urgent unmet medical need.
You’re focusing on developing small-molecule drugs for pain management. What are these and how do they work?
Small-molecule drugs are relatively simple chemicals that can enter cells easily because of their size. Once inside a cell, such drugs can interact with other molecules, like proteins, and affect how cells function. Aspirin and statins are examples of small-molecule drugs. For diabetic neuropathic pain, we want to develop small molecules to treat damaged nerve cells causing the pain.
Why focus on small-molecule drugs?
Small-molecule drugs offer several advantages over more complex types of medications. First, small molecules usually don’t have to be given intravenously or by injection; they can often be taken by mouth in pill form. Second, small-molecule drugs are often cheaper to manufacture. Third, because small molecules are relatively easy and inexpensive to prepare, more of them can be screened as potential drug candidates. A greater number of “shots on goal” increases the chance of finding a successful treatment.
What are Kv7 channels? Why do you think that activating Kv7 channels would relieve pain associated with diabetic neuropathy?
Nerve cells communicate with other nerve cells, the brain, muscles, and glands using electrical impulses. Kv7 channels are molecular gateways, or channels, that control the electrical activity of nerve cells by changing the flow of potassium in and out of cells. Potassium channels such as Kv7 affect how nerves transmit signals from a painful stimulus and how you perceive pain.
Kv7 channels exist in the areas of the body where nerve cells tend to become hyperactive, both in the central nervous system — your brain and spinal cord — and in the peripheral nerves elsewhere in the body.
Diabetes damages neurons and makes them hyperactive. Increased electrical activity in neurons can cause the symptoms of neuropathic pain. By activating specific Kv7 channels in neurons using a small-molecule drug, we hope to increase the flow of potassium to calm the hyperactive state of a nerve cell and restore normal levels of electrical activity. This “braking” action could reduce or eliminate the sensation of pain.
There’s a whole family of Kv7 channels, but our project is focusing on Kv7.2/3 channel subtypes.
Why focus on Kv7.2/3 activator specifically? What’s special about this target?
We know from several animal models of neuropathic pain that increasing Kv7.2/3 channel activity calms hyperactive neurons, reducing responses to a painful stimulus. This strengthens our hypothesis that these channels represent a promising target for treating pain in humans.
We think that a pain medication that targets Kv7.2/3 would be effective for treating neuropathic pain caused not only by diabetes, but also by traumatic injury, surgery, HIV infection, and chemotherapy. It would also be non-addictive.
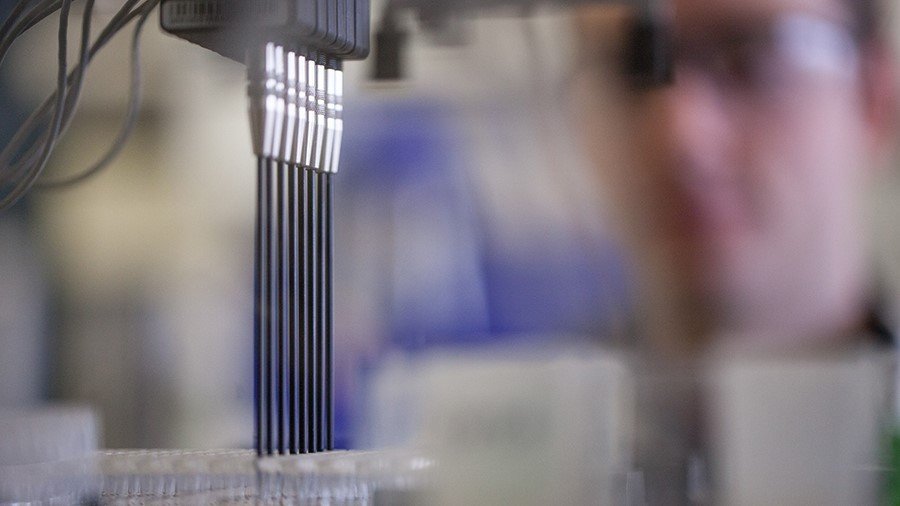
Automated liquid handling systems prepare drug candidates for testing. Titanium tips transfer compounds to 96-well plates where they are diluted to appropriate doses for testing on the Kv7.2/3 cell line. Image courtesy of Knopp Biosciences LLC
What is your team’s approach to designing a new drug to treat pain?
Our approach for discovering a new treatment for pain relies on two disciplines working closely together:
- Medicinal chemistry: Our medicinal chemists design and synthesize potential new medicines (drug candidates).
- Biological assay screening platforms: Our biologists test the drug candidates in screening assays. These assays confirm that a drug candidate activates our target, the Kv7.2/3 channels of nerve cells, without activating other Kv7 channels that could cause unwanted side effects.
As we identify promising compounds in screening assays, we then test them in other assays to predict whether they will remain intact after they are given orally to animals, and that they meet certain safety requirements. When compounds pass this stage of evaluation, we then test them in animal models of neuropathic pain.
At each step, biologists give feedback to chemists so they can optimize compounds to make them as specific as possible to Kv7.2/3 channels, reduce any unwanted side effects, and optimize other properties related to metabolism and dosing. Eventually, we select the most promising candidate and consult with the FDA to carry out clinical studies to check the candidate’s safety and effectiveness in humans.
How is NIH HEAL Initiative support making this research possible?
NIH HEAL Initiative support has been key for our efforts to develop Kv7.2/3 activators for the treatment of pain. The initiative not only provides funds for our program, but also expertise in drug discovery and the field of pain management. We meet monthly with our NIH colleagues to review our project and receive valuable advice regarding program planning and execution.
The combination of our financial resources, our respective expertise, and, importantly, our shared commitment to an important health goal, makes this project an effective public-private partnership.
What impact will this project have if successful?
If our project meets milestones as outlined in our NIH HEAL Initiative grant, we could have support from the initiative for up to five years. Within that time, we hope to discover an effective, non-addictive compound that reduces pain when tested in animal models.
After rigorous safety testing in animals, the compound would advance to the next step: human clinical trials. If human trials show the new drug is safe and effective for managing neuropathic pain, the FDA could approve it so that it is available for people who need a non-addictive alternative to opioid medicines for neuropathic pain.
Read About This Project on NIH RePORT
Learn more about this project, “Selective Kv7.2/3 activators for the treatment of neuropathic pain."

Find More Projects in This Research Focus Area
Explore programs and funded projects within the Preclinical and Translational Research in Pain Management research focus area.

National Institute of Neurological Disorders and Stroke (NINDS)
Learn more about NINDS’ role in the NIH HEAL Initiative.
 U.S. Department of Health & Human Services
U.S. Department of Health & Human Services
