
HEAL is funding research to develop and test new treatments for pain associated with sickle cell disease.
One of the hallmark symptoms of sickle cell disease is severe pain that often occurs in intense bouts called crises that can be triggered by dehydration, cold or warm temperatures, or certain foods. These episodes begin in infancy or early childhood and can persist throughout life. A pain crisis can send a person to the hospital for pain medications or blood transfusions, thus children and teens with sickle cell disease often miss school. Young adults with sickle cell disease who want to begin living independently must constantly be aware of their limitations when they go to college or begin a job.
For many people with sickle cell disease, opioid medications are a lifeline: the only way to keep pain to tolerable levels. But more choices for pain relief are welcome, and the Helping to End Addiction Long-term® Initiative, or NIH HEAL Initiative®, is funding research to develop and test new treatments for pain associated with sickle cell disease in animal models and early human studies and in clinical trials. As part of these programs, HEAL-funded researchers are testing whether complementary and integrative treatment approaches can help people with sickle cell disease better manage their pain. Other scientists are developing a novel strategy to relieve sickle cell pain by using highly focused ultrasound stimulation of the brain.
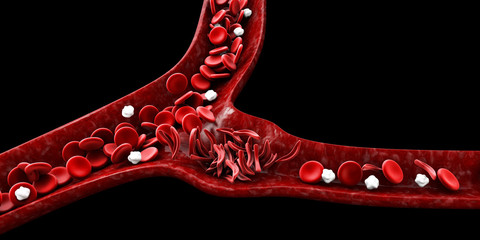
Misshapen sickle red blood cells starve cells of oxygen, which causes pain.
What Causes Sickle Cell Disease Pain?
In the United States, most people with sickle cell disease are identified right after birth through general newborn screening programs. This helps families learn about the disease, what to expect, and how to better deal with it right from the beginning.
Children and adults with sickle cell disease carry a genetic mutation in the gene for hemoglobin, the protein in red blood cells that carries oxygen from the lungs to tissues and organs. Because of the altered hemoglobin, red blood cells in these individuals are misshapen. Instead of looking like smooth, round discs, the red blood cells resemble a crescent moon or sickle and tend to clump together. As a result, the misshapen cells can’t transport oxygen as well, starving tissues and causing fatigue. Clumps of sickle cells can also clog small blood vessels, leading to crises with severe sharp, stabbing, intense, or throbbing pain.
Even with the best management, living with sickle cell disease is physically, mentally, and emotionally draining. New treatment approaches are needed – and some innovative approaches are on the horizon.
Using Complementary and Integrative Approaches to Manage Pain
Ardith Z. Doorenbos, Ph.D., R.N., and her team at the University of Illinois, Chicago, have long focused on improving pain management for people with diverse underlying conditions, including people receiving dialysis or those with cancer pain. The question is whether complementary and integrative therapies can provide an additional option beyond opioids for relief from severe pain.
For people with sickle cell disease, the researchers will evaluate two complementary and integrative treatment approaches – guided relaxation and acupuncture – both of which worked to relieve pain in initial studies. The researchers will compare the effectiveness of both approaches for relieving pain and for reducing opioid use. Participants will be randomly assigned to one of three groups, and all groups will continue to receive usual clinical care for people with sickle cell disease (which in most cases involves opioid therapy):
- Usual care
- Usual care and acupuncture
- Usual care and guided relaxation using an app
This HEAL-funded research will adapt to how people respond to their assigned treatment. After 6 weeks, participants will be asked about changes in their pain levels. Those whose pain levels have remained high will either be asked to continue the treatment for another 6 weeks to see if longer exposure to the treatment makes a difference, or they will be offered the other treatment to see if that works better.
Doorenbos’ approach, known as a pragmatic clinical trial, reflects what happens in everyday clinical practice, she explains. “If a patient doesn’t respond to the initial treatment I prescribe, I may encourage them to continue for a bit longer, or I may offer them an alternative that might work better for them because it is better suited to their preferences and lifestyle.”
The study is going on in three different healthcare systems in Illinois, North Carolina, and Florida to determine how easy it is to implement in different real-world settings. Doorenbos and her team have talked to clinic staff as well as various other collaborators – from hospital administrators and social workers to patient advocacy groups – to refine the study at each of the different sites. They are currently recruiting people who have sickle cell disease to participate.
Doorenbos acknowledges that there is currently a role for opioids in treating pain in patients with sickle cell disease, but more tools are welcomed by providers and patients alike.
Disrupting Pain Circuits in the Brain
Another novel approach to treating severe pain, including that caused by pain crises, involves technology. Bin He, Ph.D., at Carnegie Mellon University, Pittsburgh, and his team are also looking for new, non-opioid approaches for treating sickle cell disease pain, but they are at a much earlier stage in the research process. They are studying whether a device that emits highly focused ultrasound waves and targets them at specific brain regions can relieve pain in a mouse model of sickle cell disease.
Most of us are familiar with ultrasound being used as a diagnostic tool by clinicians to generate images of the body – for example, during pregnancy. However, He and his team had previously discovered that focused ultrasound waves could selectively interfere with the firing of specific nerve cells in rats’ brains.
They are looking to see if focused ultrasound waves targeted at specific brain areas only a few millimeters wide could change the activity of nerve cells that create and spread pain signals. The NIH HEAL Initiative made it possible for He and his team to pursue this work, which could be applicable to other types of pain.
Using a mouse model of sickle cell disease pain, the scientists are directing highly focused ultrasound waves at brain regions known to be part of pain circuits. Early results showed that the approach is promising; the highly focused ultrasound waves reduced animals’ sensitivity to pain.
Before such experiments can be tried in people with sickle cell disease pain, the researchers need to repeat the results many times and also show that the technology is safe: first in larger animals and then in human research participants.
The ultimate goal, He explains, is a light-weight device that people can wear to deliver focused ultrasound for about 10 to 20 minutes every day.
More Research is on the Way
In addition to these two promising research directions, the NIH HEAL Initiative will support more research under two programs aiming to increase the number of treatment options available to people with sickle cell disease.
One of these programs will focus on studies like Doorenbos’ research that evaluate novel pain treatment approaches in real-world conditions and assess how such treatments can be implemented into clinical practice. The second program will evaluate the effectiveness of diverse pain management approaches, as well as their impact on a patient’s function, overall well-being, and quality of life – including effects of stigma and other social factors that may affect quality of care.
Only by expanding the menu of treatment options available to people with sickle cell disease can their pain and suffering be diminished or eliminated entirely.
“We need more tools, more options in our toolbox so that for each patient we can find the one that works best,” says Doorenbos.
Explore Projects in These Research Focus Areas
Explore programs and funded projects within the Clinical Research in Pain Management and Preclinical and Translational Research in Pain Management research focus areas.
Read About These Projects on NIH RePORT
Read about the study led by Dr. Doorenbos. Read about the study led by Dr. He.
National Center for Complementary and Integrative Health (NCCIH)
Learn more about NCCIH’s’s role in the NIH HEAL Initiative.
National Institute of Biomedical Imaging and Bioengineering (NIBIB)
Learn more about NIBIB’s role in the NIH HEAL Initiative.
 U.S. Department of Health & Human Services
U.S. Department of Health & Human Services
