How health care providers respond to patients’ descriptions of their pain ultimately determines how that pain is managed.
An innovative project hopes to shine a light on how health care providers assess their patients’ risk of opioid misuse, with the goal of improving pain management as part of the national response to the opioid crisis.
Funded as part of the Clinical Research in Pain Management program of the Helping to End Addiction Long-term® Initiative, or NIH HEAL Initiative®, this study highlights the role of medical professionals in addressing the opioid epidemic and reducing disparities in pain care.
Doctors participating in the study log in to a computer simulation program where they “meet” animated virtual patients of different races and health histories, each of whom has an opioid prescription for chronic pain, explained Adam T. Hirsh, Ph.D., associate professor of psychology in the Purdue School of Science at Indiana University–Purdue University Indianapolis and principal investigator of the project.
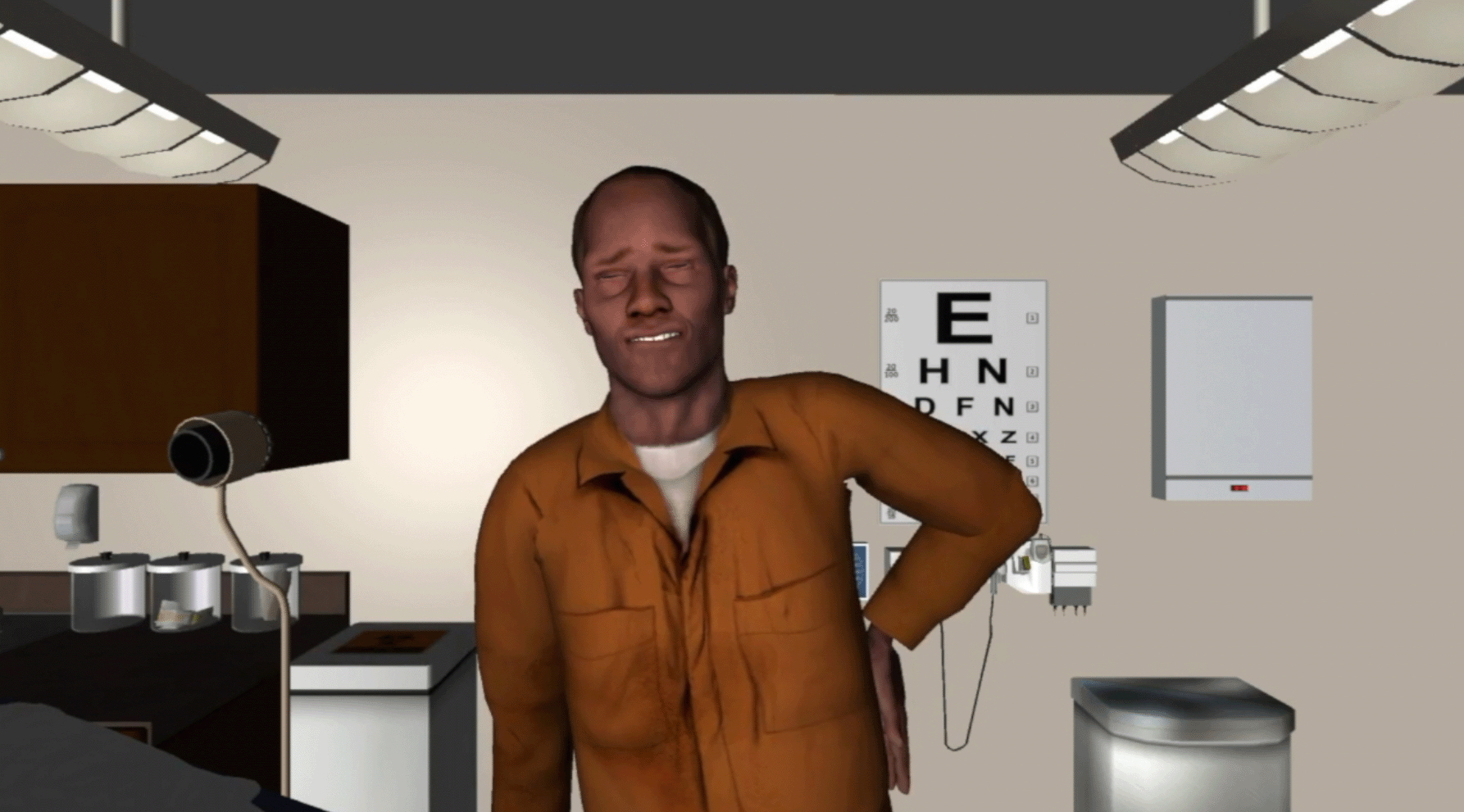
A computer-simulated patient who has back pain. Image courtesy of Adam Hirsh, Ph.D.
In some of the simulations, the patients will have taken their medicines exactly as prescribed. In others, the doctors will learn that the patients have not used their medicines as prescribed. For example, maybe they ran out of their prescription early, a sign that the patients might have taken extra doses.
Each doctor will go through similar scenarios with a total of eight different virtual patients. Just as in real life, the doctors must assess the patient’s risk of not using opioids as prescribed, misusing them, or becoming addicted. Then, the doctors will decide whether to continue the opioid prescription, reduce the dose over time, or stop it completely.
At the end of the simulation, Hirsh and his team will be able to see whether the doctors’ evaluations for potential opioid misuse and treatment decisions were influenced by the virtual patients’ race or income level. Eventually, data collected from 135 doctors participating in the project would help design a solution to reduce racial or socioeconomic biases in the treatment of patients with chronic pain.
The root of the problem
People of all races and income levels suffer from chronic pain; but their doctors are far more likely to be white and have higher incomes.1 This contrast can lead providers to make false assumptions or judgments about patients and create inconsistencies in treatment decisions.
Do these judgments and assumptions, called provider bias, create disparities in pain care? If so, how can providers overcome their biases as they assess patients’ risk for opioid misuse and recommend treatments for their pain? These are questions that Hirsh and his colleagues are trying to answer with their computer simulation project.
“Black patients in particular are less likely to receive guideline-based pain treatment, perhaps because their providers perceive them as being riskier in terms of the potential for misuse and addiction,” Hirsh said.
Expanding on a proven intervention with NIH HEAL support
Hirsh’s project for the NIH HEAL Initiative uses a modified version of a simulation program he previously developed for a study supported by the National Institute on Minority Health and Health Disparities (NIMHD), part of the National Institutes of Health. He is building on evidence from that study, in which he found that when making treatment decisions, about half of the doctors showed bias against black or economically disadvantaged patients. Such bias led to unequal treatment of pain based solely on the virtual patients’ race or socioeconomic status (SES), he found.2
“Health care providers are the gatekeepers for pain treatments, but evidence-based, provider-focused interventions to decrease bias and reduce health care disparities are rare,” Hirsh said. By adapting the simulation for the HEAL project, he says, “we hope to learn how providers are assessing their patients’ risk for misusing opioid medications and whether bias plays a role in those risk assessments.”
Helping providers do the right thing
Previous studies from this group included a follow-up intervention for the providers who showed bias in their treatment decisions. First, providers received feedback about how their treatment decisions varied, based on the virtual patients’ race or SES. Then, the providers went through a series of simulated interactions with virtual patients that included short videos showing how pain limited the patients’ enjoyment of life and their abilities to perform everyday activities. These scenarios helped the doctors see the world through their patients’ eyes, “leading to more compassion and a greater understanding of the lived experience of the other person,” Hirsh said.
Hirsh found that this type of intervention — helping doctors learn from their biases and empathize with patients living with pain — successfully reduced treatment bias against virtual patients who were black (85 percent reduction in bias) or had low SES (76 percent reduction).2
“Initially, I was concerned that providers would be defensive or resistant to feedback,” Hirsh said. “However, it turned out that providers were very open to learning about their treatment behaviors.”
Hirsh expects that the HEAL-funded project will show whether bias plays a role in how providers judge patients’ risk of misusing opioids3 and how these judgments affect their treatment decisions.
“Results from our first study show that providers do assess risk differently based on race and previous use of prescription opioids,” Hirsh said. His team is currently analyzing the data on how providers treated these virtual patients; in particular, how they managed the patients’ current opioid prescriptions and what non-opioid treatments they recommended.
“We will then be able to use these risk-assessment and treatment results to design an intervention to try to help health care providers recognize and overcome their bias to ensure that people living with chronic pain receive appropriate care,” Hirsh said.
References
1. Diversity in Medicine: Facts and Figures 2019. AAMC. https://www.aamc.org/data-reports/workforce/report/diversity-medicine-facts-and-figures-2019. Published 2019. Accessed April 9, 2020.
2. Hirsh AT, Miller MM, Hollingshead NA, Anastas T, Carnell ST, Lok BC, Chu C, Zhang Y, Robinson ME, Kroenke K, Ashburn-Nardo L. A randomized controlled trial testing a virtual perspective-taking intervention to reduce race and socioeconomic status disparities in pain care. Pain. 2019;160(10):2229–2240.
3. A manuscript based on the NIH HEAL Initiative project has been accepted for publication in American Psychologist.

Read About This Project on NIH RePORT
Learn more about Hirsh’s project, “Virtual Perspective-Taking to Reduce Race and SES Disparities in Pain Care.”

Find More Projects in This Research Focus Area
Explore research programs and funded projects within the Clinical Research in Pain Management focus area.

National Institute of Neurological Disorders and Stroke (NINDS)
Learn more about NINDS’ role in the NIH HEAL Initiative.
 U.S. Department of Health & Human Services
U.S. Department of Health & Human Services
