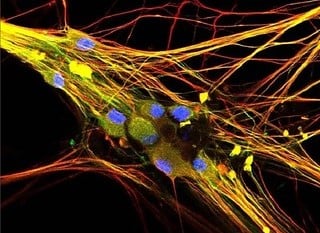
Image: NCCIH/NIH
Chances are high that someone you know is affected by chronic pain—roughly 20 percent of adults in the United States experience chronic pain. However, pain treatments are limited, can be risky, and don’t work for all types of pain, creating an urgent need for new pain management strategies.
Animal models play a critical role in understanding conditions and preliminary safety and efficacy data that allow researchers to progress to in-human trials. Animal models have their limitations, however. “There are important, pain-relevant species-to-species differences in cell physiology that can’t be ignored,” says Bryan Black, Ph.D., from the University of Massachusetts Lowell. He goes on to state that, “it is increasingly clear that sensory neuron cell types—here meaning groupings based on transcript co-expression—are not well-conserved across species, suggesting that some types of sensory neurons and nociceptors contributing to chronic pain in rodents aren’t present in humans at all.”
Through the Helping to End Addiction Long-term® Initiative, or NIH HEAL Initiative®, the National Institutes of Health is funding investigators like Black who are developing new models for testing pain treatments that better reflect human biology to expand the toolbox researchers have to investigate solutions to the complex problem of pain.
New Strategies for Answering Old Questions
Human-based models and cell culture systems that can more reliably identify promising new treatments for pain are urgently needed. Black, like other researchers, uses human induced pluripotent stem cells (hiPSCs) to study human nerve cells. Like other types of stem cells, hiPSCs can transform into many cell types found in the body. However, this type of stem cell is unique because it is created in the laboratory. To make hiPSCs, researchers collect human blood or skin cells and then reprogram them to behave like stem cells. Black transforms hiPSCs into nerve cells and their support cells, called glial cells, and uses them to create a 3D model of pain sensing on a chip. The chip detects the electrical impulses the nerves produce in response to harmful stimuli.
This chip system is used to screen for compounds that could be used as pain relievers. If the electrical impulses to harmful stimuli are changed in the presence of one or more of these compounds, the compound can be considered a “hit” worthy of further investigation. The team hopes to find compounds that, alone or in combination, reduce the baseline activity and excitability of nerve cells like the ones in the 3D model, which could eventually give people with chronic pain conditions some relief.
Donor tissue is another source of human nerve cells that can be used in pain research. These tissues come from organ donors after their death and people experiencing chronic pain who undergo surgery that requires nerve cell removal. HEAL grantees within the Program to Reveal and Evaluate Cells-to-Gene Information that Specify Intricacies, Origins, and the Nature of Human Pain (PRECISION Human Pain) network are using donor tissue samples to gain a better understanding of the cells involved in human pain processing.
Wenqin Luo, M.D., Ph.D., is the head of the Human PRECISION Pain Center at the University of Pennsylvania. Her research team studies the trigeminal ganglion, a cluster of nerve cells in the head that allows for sensation of the face and jaw. It’s also involved in headache disorders like migraines. Luo’s team uses a laser-based dissection technique to isolate single cells from trigeminal ganglia from postmortem donors. Her team then performs single cell RNA sequencing on the isolated cells to get an overall survey of the activity going on within. They also compare cellular activity in different areas of the nerve cell cluster through a process called spatial transcriptomics. Lastly, they compare the results of these techniques between postmortem donors with and without a history of migraine disorders. With this information, they hope to identify molecules or entire signaling pathways that are altered under migraine conditions, which could allow for the identification of targets for new migraine medicines.
The Integrated Research Center for Human Pain Tissues at Washington University, another branch of the PRECISION network, is working to answer similar questions. The team, led by Robert Gereau, Ph.D., studies dorsal root ganglion (DRG) cells, which are clusters of nerve cells that extend outward from the spinal cord all the way to fingers or toes. They are triggered in response to painful stimuli, like a hot pan or a sharp object, and send messages to the brain about the painful stimulus. Neuropathies happen when nerves like DRG cells are damaged. Gereau collects DRG cells from donors with and without a history of chronic pain. Among other metrics, his team measures the electrical properties of DRG cells to determine if there are any differences based on pain history. In all, this work can provide the critical clues needed to bring what researchers learn in the laboratory to the clinic.
Hope for the Future
Despite the complexity of human pain, there are several promising directions and developments on the horizon to better support people living with pain. This includes progress toward first-in-human clinical testing by submitting an investigational new drug application to the U.S. Food and Drug Administration for a small molecule inhibitor to treat chronic neuropathic (nerve) pain. The future of pain management is bright with researchers exploring therapies on many fronts.
“People who experience chronic pain are highly underserved by currently available treatments,” says Theodore Price, Ph.D., a HEAL grantee in the PRECISION network at the University of Texas Dallas. “We owe it to them to capitalize on recent technological advances that allow us to study big questions in this field and move toward therapeutic development.”
William Renthal, M.D., Ph.D., heads the PRECISION Human Pain Center at Harvard Medical School. “One of the most exciting aspects of the research occurring at our center is that it has the potential to link the perception of pain people report to the exact molecules that contribute to their pain,” Renthal says. “This critical advancement allows us to compare these new human data to mechanistic studies conducted in animal models, which increases our ability to predict which targets are most likely to yield effective pain treatments. This is an exciting time in pain medicine and research and provides genuine hope for people suffering from chronic pain and headache disorders.”
Sign Up to Receive HEAL Research News
Subscribe to receive NIH HEAL Initiative research advances in your inbox.
 U.S. Department of Health & Human Services
U.S. Department of Health & Human Services
