
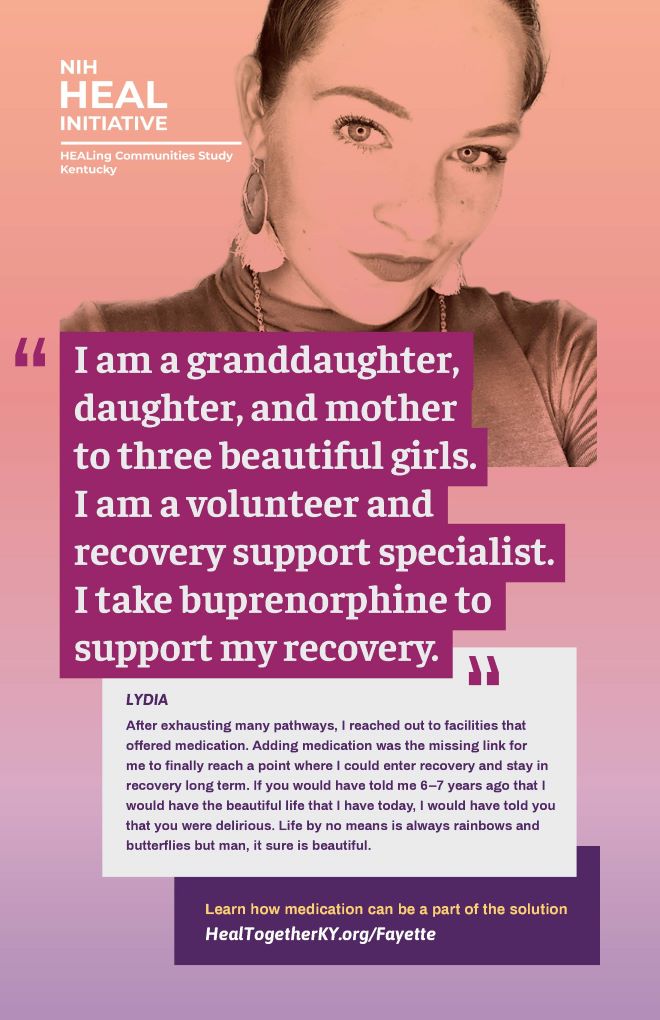
The HEALing Communities Study is using tailored communication campaigns to increase demand for naloxone. Credit: NIH HEAL Initiative
Nothing could have prepared Shelley Elswick for that surreal moment during a February 2010 ice storm: driving in the middle of the night to bail out her 18-year-old son Alex from jail.
One moment Alex had been a high-achieving student athlete in his first year of college. The next, it seemed, her son was expelled from school and stuck in a jail cell arrested for selling drugs. Yet that dark journey was only the first of many surreal moments in Shelley’s relentless back-and-forth struggle to support her son as he moved toward recovery.
“When addiction happened to my family, I was totally unprepared,” Elswick says, explaining that she was frantic, didn’t know where to go for information, and was never told about FDA-approved medications for opioid use disorder. Alex would go on to seek treatment for his addiction seven times and experienced many life-threatening relapses.
Ten years later, Alex is now in recovery. He and his mother founded Voices of Hope, a recovery community organization in Lexington, Kentucky that is partnering with the HEALing Communities Study, funded as part of the Helping to End Addiction Long-term® Initiative, or NIH HEAL Initiative® as part of its translation of research to practice for the treatment of opioid addiction. Through this study, the Elswicks and thousands of community members across the country — connected to the opioid epidemic in one way or another — are working hard to reverse its course.
Communities in need of healing
To help families like the Elswicks get access to high-quality, effective treatment, the National Institutes of Health and the Substance Abuse and Mental Health Services Administration launched the HEALing Communities Study. This research is being conducted within some of the states hit hardest by the opioid epidemic: Kentucky, Massachusetts, New York, and Ohio.
The study’s goal is ambitious but urgently needed: to reduce opioid-related overdose deaths in participating communities in these four states by 40% in three years. Although many types of opioids can lead to overdoses, illicit and extremely potent synthetic opioids like fentanyl account for the majority of opioid-related deaths in the United States.
“Overprescribing of opioids created fertile ground for opioid misuse, and then fentanyl hit us hard,” says Jeffrey Samet, M.D., of Boston Medical Center, Massachusetts, who leads the Massachusetts HEALing Communities Study project.
The HEALing Communities Study stands out in a special way: as an innovative team effort powered by people in communities who are deciding how to implement solutions that work in their own backyard. Along with the Elswicks, many individuals and organizations are playing a direct role in figuring out how to save the lives of friends and family (see “Voices from the HEALing Communities Study”).
“This research is similar to the concept of personalized medicine,” says Rebecca Jackson, M.D., of The Ohio State University, Columbus, who is leading the Ohio project.
“Every community is different: each needs effective interventions at the right time and in the right place.”
Community coalitions are working with HEALing Communities Study researchers on strategies to confront stigma. Credit: NIH HEAL Initiative
Powered by people
The HEALing Communities Study is guided by individual communities through coalitions composed of local leaders, healthcare providers, and individuals with “lived experiences” including family members, people with opioid use disorder, and those who are in recovery. Understanding both victories and struggles experienced by people like Alex and Shelley Elswick provide critical information for the research team.
As well, primary care offices, emergency departments, jails, drug or opioid courts, homeless shelters, and other organizations across the local healthcare and treatment system are working together to conduct the study.
The HEALing Community’s main research activity is to test whether a community-engaged approach — Communities that HEAL — can decrease opioid-involved deaths in several dozen communities across the four participating states with a “menu” of evidence-based options. After each community chooses a handful of these strategies to test, the study team will implement that group of approaches, then collect data to see how effective the whole set is (when packaged together) in reducing opioid-related overdose deaths. The choices include one or more each of research-backed practices including education about naloxone (Narcan®) and overdose, medication to treat opioid use disorder, and safer prescribing and use of opioids.
The researchers will collect and analyze data about which approaches worked, where, and how well. Those results can guide communities across the nation to replicate successful strategies, saving even more lives. An important element of the whole effort is development of tailored communication campaigns to increase demand for the overdose antidote naloxone, treatments for opioid use disorder, and effective safe-prescribing practices.
Fighting stigma to save lives
Pervasive stigma against people with addiction is a major barrier to recovery, and it affects nearly every aspect of substance use disorder: from prevention to diagnosis to accessing evidence-based treatments and lifesaving antidotes. Community coalitions are working with HEALing Communities Study researchers in a range of ways, including coming up with strategies to confront stigma in their communities.

Ryan Caldwell
talks about
breaking the silence
about stigma
and substance use.
Stigma can be internalized — experienced by a person with opioid use disorder — as well as held by many others within families and in community settings.
New York project leader Nabila El-Bassel, Ph.D., of Columbia University, New York City, notes that stigma can arise not only about drug use but also about racial injustices in our society toward people of color. Stigma about substance use can be compounded when it intersects with other pervasive forms of discrimination, like racism.
“Stigma is a problem for most people seeking help for opioid use disorder, but it’s a triple threat for many people of color who use drugs,” she explains.
El-Bassel says that it’s especially important to ensure that community coalitions pay attention to the unique needs of people of color and the inequities these communities face in accessing evidence-based practices to address opioid use disorders. Approximately one-fifth of the people in the New York HEALing Community Study locales are Black/African American or Hispanic/Latinx, providing opportunities to listen to these important community voices.
Stigma within the healthcare system is also a challenge. Finding doctors who will prescribe these medications and pharmacists who will fill prescriptions can be difficult. Likewise, access to naloxone is limited in some states, some of which require a prescription for it. Like with medications to treat opioid use disorder, some physicians are reluctant to prescribe naloxone, and some pharmacies do not keep it in stock.
“It’s a myth that Narcan enables drug use in people with opioid use disorder,” says Sharon Walsh, Ph.D., of the University of Kentucky School of Medicine, who leads the Kentucky project of the HEALing Communities study.
“What it does is it let people live to see another day.”
Coping with new realities
The COVID-19 pandemic occurred in the United States a few months after the HEALing Communities Study began to introduce locally chosen sets of strategies into participating communities. The communities rapidly introduced virtual health approaches through videoconferencing and other remote-delivery strategies – many had been using these technologies already throughout the planning stages of the research.
Yet isolation and access to in-person treatment was restricted due to pandemic-related closures and physical distancing recommendations. These restrictions put people at high risk for relapse or overdose.
The HEALing Communities Study leveraged its community partnerships to fast-track distribution of naloxone. Community coalitions worked with research teams to enhance availability and access to naloxone to individuals most at risk of overdose, including people being released from prison and jail because of COVID-19.
Some communities took the lead in finding creative ways to meet people where they are, safely, to provide naloxone. This included distribution at gas stations, in supermarkets — even at beaches after they had re-opened when conditions on the ground were deemed safe. Study scientists are collecting data about effects of these strategies on increasing the number of people accessing naloxone.
Despite many effective tools to reduce opioid-related overdose deaths, far too many Americans continue to die. The HEALing Communities Study is poised to identify much needed strategies to increase access to evidence-based treatments in ways that are responsive to local needs.
This scientific knowledge is using the power of people to help other communities make life-saving treatments more widely available for everyone who deserves them.
Editor’s note: This story is the first in a two-part series about the HEALing Communities Study. Next up: Voices from the Community


Find More Projects in This Research Focus Area
Explore programs and funded projects within the Translation of Research to Practice for the Treatment of Opioid Addiction research focus area.

National Institute on Drug Abuse (NIDA)
Learn more about NIDA’s role in the NIH HEAL Initiative.
 U.S. Department of Health & Human Services
U.S. Department of Health & Human Services
